Abstract
Background:
Anaplastic Large Cell Carcinoma (ALCL) is a rare form of Non-Hodgkin Lymphoma. The incidence of ALCL, especially of breast implants, has been increasing over the years. We utilized the NCDB database to study prognostic variables for ALCL, to create the largest and most comprehensive cohort of patients with primary ALCL, to analyze primary anatomical site and other prognostic variables and how they affect survival so as to help improve clinical outcomes across the world.
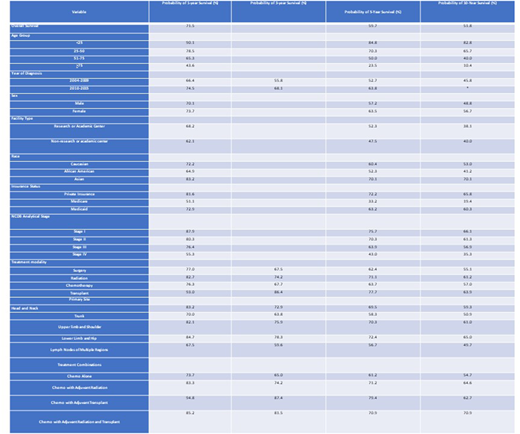
Methods: Utilizing the National Cancer Database, 3,298 patients with primary T-cell anaplastic large cell lymphoma were identified by the histology code 9714 and grade code 5. Kaplan-Meier curves and survival tables were created to calculate 1-, 5-, and 10-year survival probabilities for variables including stage, race, sex, facility type, age, insurance, primary site, year of diagnosis, and adjuvant therapy. Log-rank analysis was used to compare the groups within each variable.
Results: The cohort consisted of 61.2% male patients and 77.9% Caucasian patients with a median age of diagnosis of 51 years old. Approximately 67% of the patients were diagnosed with ALCL between the years of 2010 and 2015. The most common type of insurance was private insurance with 49.4% of the cohort followed by Medicare with 27%, Medicaid with 12.8% and not insured with 6.3%. Most patients (27.3%) were treated at academic or research facilities, closely followed by comprehensive community cancer programs with 26.4% of the cohort. The most common primary anatomical site was lymph nodes of multiple sites consisting of 34.4% of the cohort. Stage IV was the most common stage consisting of 31.8% of the cohort.
Overall 1-, 5-, and 10-year survival probabilities for patients with ALCL were 71.5%, 59.7%, and 51.8%, respectively. As age increased, overall survival decreased, with the ≥75 age group having the worst 1- and 5-year survival probability of 43.6% and 23.5%, respectively. Patients diagnosed between the years of 2004-2009 (1-year:66.4% and 5-year:52.7%) had much worse survival probabilities when compared to patients diagnosed between the years of 2010-2015 (1-year:74.5% and 5-year:68.1%). Caucasian patients had better 1-,5- and 10-year survival outcomes when compared to African Americans with 1-year survival probabilities of 72.2% and 64.9%, respectively. Facilities other than research or academic centers and Medicare or Medicaid insurance had worse 1-,5-, and 10-year survivals when compared to research or academic centers and private insurance. As stage increased, overall survival probabilities decreased. The lower limb and hip anatomical site had the best survival outcomes with 1- and 5-year survival probabilities of 84.7% and 78.3% respectively. Adjuvant hematologic transplant patients did best with a 1- and 5-year survival probabilities of 94.8% and 87.4%, respectively, followed by an adjuvant combination of both radiation and hematologic transplant (1-year:85.2% and 5-year:81.5%), adjuvant radiation (1-year:83.3% and 5-year:74.2%), and chemotherapy alone (1-year:73.7% and 5-year:65.0%).
DISCUSSION:
This is the largest and most comprehensive study to date on the epidemiology and prognostic factors of Anaplastic Large Cell Lymphoma. The results of our analysis bring up several interesting trends, the most interesting one being the marked increase in survival rates between 2010- 2015 compared to 2004-2009. This is likely attributed to better treatment modalities. With regards to treatment modalities, patients who underwent chemotherapy followed by adjuvant transplant had better 1, 3, 5 and 10 year survival rates compared to all other treatment modalities. As previously established, younger age at diagnosis is a good prognosis factor. Other major factors influencing survival, previously unstudied, are facility type, race, insurance status, stage, adjuvant therapy, and primary site. Asians and those with private insurance had better survival rates. Primary site involving multiple lymph nodes carried the worst prognosis, while lower limb and hip as primary sites carried the best prognosis. Patients treated at academic and research center had better prognosis compared to those treated at non- academic centers. Performing a multi-variate analysis and further studies to elucidate the causes of improved survival associated with some of these factors will help improve quality of care for patients with ALCL.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.